A Stewart-Treves syndrome of the lower limb
Published Web Location
https://doi.org/10.5070/D38d1463nqMain Content
Letter: A Stewart-Treves syndrome of the lower limb
Nicola di Meo, Marina Drabeni, Alessandro Gatti, Giusto Trevisan
Dermatology Online Journal 18 (6): 14
Clinica Dermatologica, Ospedale Maggiore di Trieste, Universita’ degli Studi di Trieste, Trieste, ItalyAbstract
We report a case of a Stewart-Treves syndrome of the lower limb. The tumor is best described in the upper limb following breast cancer treatment but a small number of cases have arisen in lymphedema of the lower limb. Electrochemotherapy could be useful in the palliative treatment of this lymphangiosarcoma.
A rare but important complication of chronic lymphedema is the development of cutaneous malignancy. The best-known associated malignancy is lymphangiosarcoma [1].
The Stewart-Treves syndrome describes lymphangiosarcoma developing from well-established postmastectomy edema. However, lymphangiosarcoma is now described as occurring with lymphedema of any cause. The favored theory for these associations is altered immune surveillance in the lymphedematous region [2]. The tumor metastasizes early and has a poor prognosis. The tumor is best described in the upper limb following breast cancer treatment, but a small number of cases have arisen in lymphedema of the lower limb, or in the upper limb without breast cancer and mastectomy [3]. An 81-year-old cardiopathic woman with a history of melanoma of the left calf, treated with a radical excision and unilateral inguinal lymph node dissection in 1992, presented with a 5-month history of an enlarging ulcerated plaque of coalescing purple papules and bruise-like nodules within a region of chronic lymphedema of the left lower limb (Figure 1).
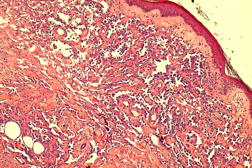
A skin biopsy of the lesion showed irregular anastomosing vascular channels lined by endothelial cells with different degrees of atypia and mitotic activity alternating with areas of closely spaced cells with a high mitotic index and spindle-like morphology (Figure 2). In this case immunohistostaining for CD31 and Ki67, vascular markers, was helpful for the establishment of the diagnosis of lymphangiosarcoma. HHV-8 staining was negative. Considering both the size of the tumor and the patient’s general condition, surgery wasn’t an option for our patient. So, we considered a palliative local electrochemotherapy regimen with bleomicin. Unfortunately the patient died from a stroke before starting treatment. Stewart-Treves syndrome is a rare complication of chronic lymphedema mainly related to breast cancer. It has also been observed in the lower extremity and can result from congenital, idiopathic, traumatic, filarial, or postsurgical causes of lymphedema [4]. The accumulation of protein-rich interstitial fluid alters the local immune response within the affected limb and stimulates lymphangiogenesis for the development of collateral vessels. Because immune surveillance is compromised, lymphedema creates an immunologically vulnerable milieu for the development of malignancy, specifically vascular tumors [5]. STS typically develops after a 10- to 15-year latency and accounts for approximately 5 percent of angiosarcomas. The prognosis is very poor with a five-year survival close to 15 percent despite the various treatment modalities [6]. The treatment of choice is a large resection, but some authors recommend radical resection in the form of disarticulation or amputation. Surgical treatment can be preceded or followed by radiation therapy. Locally advanced tumors or metastatic forms can be treated with mono or polychemotherapy, systemic or local [7]. Electrochemotherapy is an effective local tumor ablation modality in the treatment of solid cancers. Its use combines the administration of non-permeable or poorly permeable highly intrinsic cytotoxic drugs with the application of short and intense electric pulses to the tumors to facilitate the drug delivery into the cancer cells [8]. The absence of systemic side effects and the low impact on the immune system also make this treatment suitable for elderly people as palliative care, even with repeated courses [9]. Currently, the tumors most frequently treated with ECT are melanoma and breast cancer metastases, but also head and neck cancers, primary tumors of the skin, and Kaposi sarcoma [8]. This letter is intended as a reflection about the possibility of using ECT in this particular case; this application has never been reported in literature.
References
1. Stewart FW, Treves N. Lymphangiosarcoma in postmastectomy lymphoedema. Cancer 1948; 1: 64-81. [PubMed]2. Shreiber H, Barry FM, Russell WC et al. Stewart-Treves syndrome: a lethal complication of post mastectomy lymphoedema and regional immune deficiency. Arch Surg 1979; 114: 82. [PubMed]
3. Scott RB, Nydick I, Conway H. Lymphangiosarcoma arising in lymphedema. Am J Med 1960; 28: 1008-12. [PubMed]
4. Durr HR, Pellengahr C, Nerlich A, et al. Stewart-Treves syndrome as a rare complication of a hereditary lymphedema. Vasa 2004 33:42-45. [PubMed]
5. Ruocco V, Schwartz RA, Ruocco E: Lymphedema: An immunologically vulnerable site for development of neoplasms. J Am Acad Dermatol 2002; 47:124-127. [PubMed]
6. Budd GT. Management of Angiosarcoma. Curr Oncol Rep 2002 4:515 [PubMed]
7. Wierzbicka-Hainaut E, Guillet G. Stewart-Treves syndrome (angiosarcoma on lyphoedema). A rare complication of lymphoedema. Presse Med. 2010 Dec;39(12):1305-8. [PubMed]
8. Reinhold U. Electrochemotherapy for primary skin cancer and skin metastasis related to other malignancies. Anticancer Drugs. 2011 Sep;22(8):711-8. [PubMed]
9. Curatolo P, Quaglino P, Marenco F, Mancini M, Nardò T, Mortera C, Rotunno R, Calvieri S, Bernengo MG. Electrochemotherapy in the treatment of Kaposi sarcoma cutaneous lesions: a two-center prospective phase II trial. Ann Surg Oncol. 2012 Jan;19(1):192-8. [PubMed]
© 2012 Dermatology Online Journal