Cutaneous lesions as the first manifestation of systemic follicular lymphoma in an HIV patient
Published Web Location
https://doi.org/10.5070/D381k183b9Main Content
Cutaneous lesions as the first manifestation of systemic follicular lymphoma in an HIV patient
Elisabete Moreira1, Carmen Lisboa1, Sérgio Alves1, Ilídia Moreira2, Elsa Fonseca3, Filomena Azevedo1
Dermatology Online Journal 14 (7): 17
1. Department of Dermatovenereology, Hospital S. João, Porto, Portugal. elisabetedosmoreira@gmail.com2. Clinical Hematology, Hospital S. João, Porto, Portugal
3. Pathology, Hospital S. João, Porto, Portugal
Abstract
Human immunodeficiency virus (HIV) patients have an increased incidence of lymphomas, particularly when there is a significant immunosupression. Most commonly, they are non-Hodgkin B cell type with a high or intermediate grade and have an extranodal presentation. We report the case of a 38-year-old man with HIV infection who presented with a 1-year history of a painless tumor on the back and lymphadenopathies. The diagnosis of B cell lymphoma follicle center cell type was established by skin biopsy. Staging included a bone marrow biopsy revealing infiltration by the lymphoma and a whole-body computed tomographic scan showing multiple cervical and axillary lymphadenopathies with necrotic center. Biopsy of an axillary lymph node revealed caseating epithelioid granulomas and Ziehl-Neelson staining was positive for acid-fast bacilli. The patient started therapy for tuberculosis and polychemotherapy for lymphoma with complete response. This report illustrates a case of simultaneous occurrence of tuberculosis and systemic follicular lymphoma presenting in skin in an HIV patient.
Introduction
Human immunodeficiency virus patients have an increased incidence of lymphomas, being about 100 times more common than in the general population and the risk is particularly high when there is significant immunosupression.
With the advent of highly active antiretroviral therapy (HAART) there has been a dramatic decrease in the incidence of opportunistic infections and Kaposi sarcoma, but non-Hodgkin lymphoma (NHL) and Mycobacterium tuberculosis infections have decreased less, remaining a significant problem in these patients [1, 2].
Case report
 |
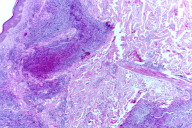
| Figure 1 |
|---|
| Figure 1. Grouped nodules on the lower back |
A 38 year-old man with HIV infection had a 1-year history of slowly progressing group of red nodules on the back in zosteriform pattern, measuring all together about 8 cm in maximum dimension (Fig. 1). Physical examination also revealed enlarged cervical and axillary lymph nodes. There were no local or constitutional symptoms. The patient had a history of herpes zoster infection, but in a different localization. The HIV infection had been diagnosed the year before and due to cutaneous drug reactions and gastrointestinal intolerance the patient was not on medication with antiretroviral drugs. A skin biopsy showed poorly defined nodular aggregates in the dermis consisting mainly of large-sized lymphoid cells (Figs. 2a & 2b). Most of these cells were CD20 positive and some of them were bcl-2 positive. Centrocytes were also present and according to cytological classification he had a follicular lymphoma grade 3a. The staging procedure included a bone marrow biopsy revealing involvement by the B cell lymphoma.
 | 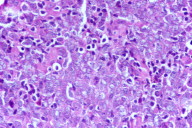 |
| Figure 2a | Figure 2b |
|---|---|
| Figure 2a. Nodular infiltrates in the dermis Figure 2b. Composed of centroblasts and centrocytes | |
Laboratory analysis revealed elevation of some parameters related to hepatic function (AST-43 U/L, ALT-11 U/L, γGT-296 U/L, FA-275 U/L). The white blood cell count was 9.4 K/mm3 (neutrophils 60.6%, lymphocytes 32.8%, monocytes 5.1%), the red blood cell count was 4.75 M/mm3, hemaglobin 14.2 g/DL and platelet count 229K/mm3. CD4 cell count was 306 mm3 and serological tests for Epstein-Barr virus were negative. Other chemistry values, including LDH, GGT2 microglobulin and protein electrophoresis were within the normal range.
A whole body computed tomographic scan disclosed multiple cervical and axillary lymphadenopathies, most of them with necrotic centers. Biopsy of an axillary lymph node showed caseating epithelioid granulomas and Ziehl-Neelson staining was positive for acid-fast bacilli. There were no signs of malignancy on that lymph node. There was no evidence of tuberculosis in other organs.
Considering the clinicopathological findings, the patient was diagnosed with AIDS, systemic follicular lymphoma staged as Ann Arbor IV A, and ganglionar tuberculosis.
The patient started therapy with a 4-drug tuberculosis regimen (isoniazid, rifampicin, pyrazinamide and ethambutol) and underwent 8 cycles of polychemotherapy (CHOP - cyclophosphamide, adriamicin, vincristine and prednisolone) with complete response of both diseases and without any major toxicity.
After 2.5 years of follow-up, the patient remains in complete remission and is now tolerating a new combination of antiretroviral drugs (lopinavir, ritonavir, and efavirenz).
Discussion
Overall, almost 3 percent of AIDS patients present with non-Hodgkin lymphoma [3]. A number of factors are likely to contribute to the high risk of lymphomas in an HIV-infected person, such as the severe and prolonged immunodeficiency, measured by CD4 cell count, the disfunction in CD4 and CD8 activity with subsequent impairment of tumor immunosurveillance, concomitant Epstein-Barr virus infection [4], and the chronic antigenic stimulation by HIV infection, leading to B cell expansion and accumulation of random somatic mutations [5, 6].
Acquired immune deficiency syndrome-related NHL are usually a late manifestation of infection by HIV and most commonly they are high grade (62%) or intermediate grade (29%) B cell lymphomas, have an extranodal presentation, and have a less favorable outcome [7]. Approximately 80 percent of all HIV-NHL are systemic.
In HIV patients, 3 histologic subtypes of NHL are more common: high grade immunoblastic, diffuse large B cell (DLBCL) and Burkitt lymphomas. Indolent B cell lymphoma represents only a small proportion of all lymphomas occurring among HIV patients.
Follicular lymphoma (FL) is generally considered an indolent NHL characterized by a follicular pattern. According to WHO classification, FL is graded into 3 categories (Grades 1-3) based on the number of centroblasts. Grade 3, having more than 15 centroblasts per high power field, is further subdivided into grades 3a and 3b. In grade 3a, centrocytes are still present and it appears to represent the aggressive end of the clinical spectrum of indolent NHL, closely related to grades 1 and 2 FL. FL grade 3b, characterized by solid sheets of centroblasts without centrocytes may be similar to DLBCL, being more aggressive [8, 9].
Tuberculosis is also increased in HIV patients and clinical features vary according to CD4 cell count. It is often characterized by an atypical course with unusual extrapulmonary disease. The presence of TB is associated with increased viral loads and more rapid progression of HIV infection. Cell-mediated immunity plays a critical role in the control of mycobacterial infections and factors that influence the cell-mediated response may facilitate the development of tuberculosis [10].
In our patient, the risk of tuberculosis was especially high due to the immunosupression caused not only by HIV infection but also by lymphoma. This report illustrates a case of simultaneous occurrence of ganglionar tuberculosis and systemic NHL. An awareness of this possible combinaton, particularly in an HIV patient, will allow physicians to make an early diagnosis.
References
1. Ledergerber B, Telenti A, Egger M. Risk of HIV related Kaposi's sarcoma and non-Hodgkin's lymphoma with potent antiretroviral therapy: prospective cohort study. BMJ 1999; 319: 23-24. PubMed2. Kirk O, Gatell JM, Mocroft A, et al. Infections with Mycobacterium tuberculosis and Mycobacterium avium among HIV-infected patients after the introduction of highly active antiretroviral therapy. Am J Respir Crit Care Med 2000; 162: 865-872. PubMed
3. Levine AM. Acquired immunodeficiency syndrome-related lymphoma. Blood 1992, 80 (1): 8-20. PubMed
4. Shibata D, Weiss LM, Hernandez AM, et al. Epstein-Barr virus-associated non-Hodgkin's lymphoma in patients infected with the human immunodeficiency virus. Blood 1993; 81: 2102-2109. PubMed
5. Shirai A, Cosentino M, Leitman-Klinman SF, Klinman DM. Human immunodeficiency virus infection induces both polyclonal and virus-specific B-cell activation. J Clin Invest 1992; 89 (2): 561-569. PubMed
6. Grulich AE, Wan X, Law MG, et al. B-cell stimulation and prolonged immune deficiency are risk factors for non-Hodgkin lymphoma in people with AIDS. AIDS 2000; 14: 133-140. PubMed
7. Ziegler JL, Beckstead JA, Volberding PA, et al. Non-Hodkin's lymphoma in 90 homosexual men: relation to generalized lymphadenopathy and the acquired immunodeficiency syndrome. N Engl J Med 1984; 311 (9): 565-570. PubMed
8. Winter JN, Gascoyne R, Van Besian K. Low-grade lymphoma. Hematology Am Soc Hematol Educ Program 2004; 203-220. PubMed
9. Ott G, Katzenberger T, Lohr A, et al. Cytomorphologic, immunohistochemical, and cytogenetic profiles of follicular lymphoma: 2 types of follicular lymphoma grade 3. Blood 2002; 99: 3806-3812. PubMed
10. Centkowski P, Sawczuk-Chabin J, Prochorac M, Warzocha K. Hodgkin's lymphoma and tuberculosis coexistence in cervical lymph nodes. Leuk Lymphoma 2005; 46: 471-475. PubMed
© 2008 Dermatology Online Journal

