mycetoma over forehead in a lepromatous leprosy patient
Published Web Location
https://doi.org/10.5070/D36px3r9zkMain Content
Nocardia nova mycetoma over forehead in a lepromatous leprosy patient
M Dhingra1 MD, N Kaistha2 MD, N Bansal2 MD, LS Solanki1 MD, J Chander2 MD DNB, GP Thami1 MD, WW van de Sande3 PhD
Dermatology Online Journal 18 (7): 3
1. Department of Dermatology, Government Medical College and Hospital, Chandigarh, India2. Department of Microbiology, Government Medical College and Hospital, Chandigarh, India
3. Department of Medical Microbiology and Infectious Diseases, Erasmus MC, Rotterdam, The Netherlands
Abstract
We present a case of a 31-year-old male, a known patient with lepromatous leprosy with a type 2 lepra reaction, who presented with a slowly growing asymptomatic swelling with multiple discharging sinuses over the forehead that developed over 6 months. Smears of the serosanguinous discharge on Gram staining showed Gram-positive branching filamentous bacilli, which on culture on blood agar showed chalky-white colonies. Histology of the lesion showed suppurative granulomas with polymorphs surrounding characteristic grains. The isolate was identified as Nocardia nova by gene sequencing and the patient was started on combined antibiotic therapy that resulted in complete resolution of the infection in six months. To the best of our knowledge, this is the first report of mycetoma related to Nocardia nova in association with leprosy.
Introduction
Primary cutaneous nocardiosis, although uncommon, may present clinically as mycetoma, lymphocutaneous infection, or acute superficial skin and subcutaneous tissue infections, such as abscess or cellulitis [1]. We here report a case of nocardial mycetoma over the forehead in a patient with lepromatous leprosy.
Case report
A 31-year-old man presented with a slowly growing asymptomatic swelling with multiple discharging sinuses on the forehead for the last 6 months. He had been receiving intermittent systemic glucocorticosteroid therapy for a type 2 lepra reaction for the last 2 years. The patient had completed the WHO multibacillary multidrug therapy (MBMDT) regimen consisting of rifampicin 600 mg once a month, clofazimine 300 mg once a month and 50 mg daily, along with dapsone 100 mg daily for lepromatous leprosy over a period of 12 months. This regimen had been completed 1 prior to presentation. He had history of trauma over the forehead in a traffic accident 5 years previously.
 |  |
| Figure 1 | Figure 2 |
|---|---|
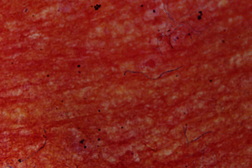
| Figures 1a and 1b. Single, ill-defined swelling with multiple sinuses over the right side of the forehead Figure 2. Gram-positive branching filamentous bacilli (Gram stain x100) | |
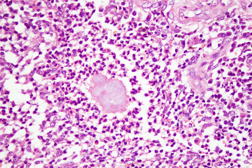
Cutaneous examination revealed a single 5 x 4 cm sized, ill-defined woody hard swelling with multiple sinuses and serosanguinous discharge over the right side of the forehead (Figures 1a and 1b). Regional lymph nodes were not enlarged. Systemic examination was unremarkable. Hematological and biochemical laboratory parameters were normal. ELISA for HIV was negative. Chest X-ray was normal. X-ray of the skull showed soft tissue swelling with no bony changes. Smears of the serosanguinous discharge on Gram staining showed Gram-positive branching filamentous bacilli (Figure 2), which were partially acid-fast on modified Kinyoun stain. Culture on blood agar showed chalky-white colonies. The isolate was further identified by 16S rDNA PCR amplification using the primers EUB-L (5′-CTTTACGCCCATTTAATCCG-3′) and EUB-R (5′-AGAGTTTGATCCTGGTTCAG-3′) according to the method of Wilson et al [2]. The resulting PCR product was sequenced and this sequence was used to search for homology in the public databases by the BLAST algorithm at NCBI (http://blast.ncbi.nlm.nih.gov/Blast.cgi). The sequence matched 100 percent with Nocardia nova. Histology of the lesion showed suppurative granulomas with polymorphs surrounding characteristic grains (Figure 3).
 |  |
| Figure 3 | Figure 4 |
|---|---|
| Figure 3. Dermis showing polymorphs and eosinophils surrounding the characteristic grains (H&E x100) Figure 4. Complete resolution after 6 months of therapy | |
The patient was given an intensive 4-week regimen consisting of intravenous gentamicin 80 mg twice daily along with oral cotrimoxazole, 320/1600 mg twice daily. Further treatment was continued with cotrimoxazole (320/1600 mg) and doxycycline 100 mg twice daily orally for the next 6 months. The lesion resolved partially after 4 weeks, with continued improvement in next few months. Complete remission was observed at the end of 6 months of therapy (Figure 4) and there was no relapse after a 1-year follow-up.
Discussion
Nocardia are aerobic Gram-positive filamentous bacilli and there are several species of clinical importance, such as N. brasiliensis, N. asteroides, N. otitidiscaviarum, and N. transvalensis. The recently recognized species, N. farcinica and N. nova, are less common causative agents for primary cutaneous nocardiosis [3].
Nocardia nova has distinct biochemical properties and is susceptible or moderately susceptible to both amoxicillin and erythromycin, but resistant to amoxicillin-clavulanic acid. Gene sequencing provides a more definitive identification and is being increasingly used [4]. There are only a few case reports of primary cutaneous nocardiosis including mycetomas by N. nova. Miller reported a case of N. nova mycetoma of the foot with bony involvement. The patient had complete resolution as in our case with prolonged antibiotic therapy [5]. Shimizu et al reported a case of mycetoma of the hand with excellent response to dapsone [6]. Other forms of cutaneous nocardiosis, such as the deep abscess and lymphocutaneous type caused by N. nova, have been reported in HIV-positive patients [7, 8].
Although leprosy and mycetoma have a similar demographic profile, there are only two case reports in the literature of mycetoma developing in leprosy patients [9, 10]. Jayakumar et al reported a case each of actinomycetoma and eumycetoma associated with leprosy [9]. In the second case report, N. brasiliensis was isolated from a mycetoma in a leprosy patient [10]. In both of these case reports, patients had anesthetic feet prone to trauma, which could have contributed to the development of mycetomas. In our patient the forehead was an unusual location for mycetoma.
Treatment of actinomycetomas is usually medical with cure rates ranging from 60 percent to 90 percent in mycetomas caused by Nocardia spp., which show a better response to drug therapy. Sulfonamides and sulfonamide combinations such as trimethoprim-sulfamethoxazole (cotrimoxazole) are usually the first-line treatments. Aminoglycosides, tetracyclines, rifampicin, ciprofloxacin, and amoxicillin-clavulanate (co-amoxiclav) have also been successfully used [11]. Welsh et al [12] used up to 4 cycles of Amikacin (15 mg/kg or 500 mg twice daily for 21 days with intervals of 2 weeks between cycles in conjunction with oral co-trimoxazole given daily during each 5-week cycle). The addition of aminoglycosides to cotrimoxazole gives higher efficacy and shorter treatment duration. This is especially advocated for use in cases at risk of pulmonary spread or vertebral involvement. Broad-spectrum agents like oxazolidinones (linezolid) and the carbapenems (imipenem) have shown efficacy particularly for the management of resistant or severe cases. Combined antibiotic therapy is preferable to monotherapy in treatment of actinomycetomas to avoid drug resistance and to eradicate residual infection [11]. Our patient showed an excellent therapeutic response to the two-step regimen as described by Ramam [13]. Our patient was immunosuppressed because he had been on long-term oral corticosteroids for treatment of a lepra reaction. For this reason we preferred to give a combination regimen to circumvent not only the emergence of drug resistance but also to prevent the systemic spread of Nocardia infection. Also, the occurrence of mycetoma in the present case, in spite of the patient having received dapsone as well as rifampicin as part of MBMDT regimen, suggests that the history of trauma received 5 years ago could have been a chance finding and actual inoculation could have been more recent. Alternatively, these drugs may have just been ineffective in the present case. Also, rifampicin in monthly doses may not have been effective, because it is given in daily doses for treatment of actinomycetomas [14].
To the best of our knowledge, this is the first report of facial actinomycetoma caused by N. nova in association with leprosy.
References
1. Dodiuk-Gad R, Cohen E, Ziv M, Goldstein LH, Chazan B, Shafer J, Sprecher H, Elias M, Keness Y, Rozenman D. Cutaneous nocardiosis: report of two cases and review of the literature. Int J Dermatol. 2010 Dec;49(12):1380-5. [PubMed]2. Wilson KH, Blitchington RB, Greene RC. Amplification of bacterial 16S ribosomal DNA with polymerase chain reaction. J Clin Microbiol. 1990 Sep;28(9):1942-6. Erratum in: J Clin Microbiol 1991 Mar;29(3):666. [PubMed]
3. Inamadar AC, Palit A. Primary cutaneous nocardiosis: a case study and review. Indian J Dermatol Venereol Leprol. 2003 Nov-Dec;69(6):386-91. [PubMed]
4. Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. 2006 Apr;19(2):259-82. [PubMed]
5. Miller SD. Madura foot: treatment of Nocardia nova infection with antibiotics alone. Am J Orthop (Belle Mead NJ). 2001 Jun;30(6):495-8. [PubMed]
6. Shimizu A, Ishikawa O, Nagai Y, Mikami Y, Nishimura K. Primary Cutaneous nocardiosis due to Nocardia nova in a healthy woman. Br J Dermatol. 2001 Jul;145(1):154-6. [PubMed]
7. Schiff TA, Sanchez M, Moy J, Klirsfeld D, McNeil MM, Brown JM. Cutaneous nocardiosis caused by Nocardia nova occurring in an HIV-infected individual: a case report and review of the literature. J Acquir Immune Defic Syndr. 1993 Jul;6(7):849-51. [PubMed]
8. Inamadar AC, Palit A, Peerapur BV, Rao SD. Sporotrichoid nocardiosis caused by Nocardia nova in a patient infected with human immunodeficiency virus. Int J Dermatol. 2004 Nov;43(11):824-6. [PubMed]
9. Jayakumar J, Aschhoff M, Renuka G. Mycetomas in leprosy. Indian J Lepr. 1993 Apr-Jun;65(2):229-33. [PubMed]
10. Kulkarni RB, Patil RT, Praveena S. Actinomycotic mycetoma due to Nocardia brasiliensis in a case of leprosy. Indian J Lepr. 2001 Jul-Sep;73(3):263-5. [PubMed]
11. Ameen M, Arenas R. Developments in the management of mycetomas. Clin Exp Dermatol. 2009 Jan;34(1):1-7. [PubMed]
12. Welsh O, Sauceda E, Gonzalez J, Ocampo J. Amikacin alone and in combination with trimethoprim-sulfamethoxazole in the treatment of actinomycotic mycetoma. J Am Acad Dermatol. 1987 Sep;17(3):443-8. [PubMed]
13. Ramam M, Bhat R, Garg T, Sharma VK, Ray R, Singh MK, Banerjee U, Rajendran C. A modified two-step treatment for actinomycetoma. Indian J Dermatol Venereol Leprol. 2007 Jul-Aug;73(4):235-9. [PubMed]
14. Damle DK, Mahajan PM, Pradhan SN, Belgaumkar VA, Gosavi AP, Tolat SN, Gokhale NR, Mhaske CB. Modified Welsh regimen: a promising therapy for actinomycetoma. J Drugs Dermatol. 2008 Sep;7(9):853-6. [PubMed]
© 2012 Dermatology Online Journal

