Tungiasis in the United States: A travel souvenir
Published Web Location
https://doi.org/10.5070/D359h843gxMain Content
Tungiasis in The United States: A travel souvenir
Jon Hager MD, Aleda Jacobs MD, Ida F Orengo MD, Ted Rosen MD
Dermatology Online Journal 14 (12): 3
Department of Dermatology, Baylor College of Medicine Houston, Texas, United States. vampireted@aol.comAbstract
Tungiasis is a cutaneous infestation caused by the burrowing flea, Tunga penetrans. This infection typically results in the development of one or more wart-like fibrous papulonodules. The causative flea is endogenous to Central and South America, sub-Sarahan Africa and portions of India; consequently, tungiasis is rarely reported in North America. However, because of increasing air travel to and from endemic areas due to business and pleasure, it is imperative that this entity remain in the differential diagnosis when evaluating clinically suggestive lesions in a patient who also has a history of recent travel. We report a case of tungiasis in a 24-year-old Caucasian woman who presented with 7-week history of a non-healing, eroded nodule on the medial aspect of her left great toe. Significant history included travel to Tanzania during three months immediately prior to presentation. Following the presumptive clinical diagnosis of tungiasis, surgical removal of the flea and its contents was performed and the base of the lesion was curetted, without complication. The specimen was sent for histopathologic correlation which confirmed the diagnosis.
Case Report
 |
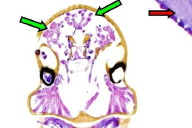
| Figure 1 |
|---|
| Figure 1. Classic Stage III lesion of tungiasis on the foot |
A previously otherwise healthy 24-year-old woman presented to our dermatology clinic with a 7-week history of a non-healing, flesh-colored scaly nodule on the medial aspect of her left great toe. The patient reported pain in the area at the onset of the lesion, but indicated that this symptom significantly diminished after a few days. Additional history unveiled a recent Peace Corps volunteer trip that included travel to Tanzania, during which the patient reported being either barefoot or wearing open-toed sandals on the beach and surrounding areas. There was no known history of trauma to the affected area. There were no other significant findings or pertinent history. Physical examination revealed a superficially eroded papulonodule with a notable central black eschar (Fig. 1). A diagnosis of Tungiasis was made on the clinical history and physical findings alone. The case was a classic presentation including a history of travel to an endemic region. Surgical deep shave excision of the flea and surrounding tissue was performed. The excision was followed by curettage and light hyfrecation (the latter designed to obtain hemostasis). The patient tolerated the procedure well and there were no complications. A histological specimen showed dermal infiltration by an ectoparasite with a thick chitinous external wall and internal structures compatible with eggs, striated muscle, and viscera (Fig. 2).
Discussion
Tungiasis is a cutaneous infectious disease caused by infestation with the insect, Tunga penetrans, also known as the sand flea or chigoe flea. In endemic locales, the disorder may be known as jiggers, nigua, or pico. This flea mainly infests humans, dogs, cats and pigs (although rats and other rodents occasionally become hosts) [1]. The earliest well documented records of T. penetrans infections in humans date back to the years of European discovery of the Americas, with the first mention being credited to an author who reported sand flea lesions from Haiti in 1525 [2]. It is recorded that this flea caused such rampant disease in some South and Central American countries that inhabitants were forced to leave their infested villages. Although the flea was originally endemic only to South and Central America, it was carried to Africa (Angola) in the 19th century in the ballast sand of an English vessel sailing from Brazil; it was first reported in India in 1899 and in the United States in 1929 in New Orleans [3].
Tungiasis is caused by penetration of the flea through an intact epidermis by the pregnant female T. penetrans. The tiny (1 mm in greatest dimension) flea then burrows deep to the epidermal-dermal junction to feed on blood from dermal capillaries. As the parasite becomes engorged, it can enlarge up to 1000-3000 times its original volume, up to a diameter of 1 cm [4]. Subsequently, the invaded local tissues become inflamed and the characteristic pain, tenderness, and swelling ensue. Within 1-3 weeks the flea extrudes hundreds of eggs that disseminate from the wound and into the environment. The exact biohabitat of the early stages of the flea are unknown. Following release of eggs, the adult dies shortly thereafter.
Patients with this condition most commonly present with a lesion on the plantar, interdigital or periungual regions of the foot, but infestations of the leg, buttocks, hand, and elbow have also been recorded [3, 5, 6]. It is likely that the foot is most often affected, in part, because the flea is a poor jumper. Handheld dermoscopy may aid in visualizing the insect's dark exoskeleton and multiple eggs within the hyperkeratotic nodule [7]. The gross appearance of the lesion varies according to the progression of the infestation process. This progression is described by the Fortaleza Classification system [4]. In stage I (early infestation; 30-120 minutes), the flea that penetrated the epidermis is visible as a reddish spot. In stage II (1-2 days), the hypertrophied flea is visible as a 1-2+ mm opalescent spot with a central dark punctum. Stage III (2-21 days) is characterized by an indurated white halo, 3-10 mm in diameter, circumscribed around a central dark punctum. Hyperkeratosis is apparent, pain is common, and extruded eggs may be visible. In stage IV (3-5 weeks), a crusty dark ring of necrotic epidermis forms around the lesion, which now contains a dead parasite. Lesional involution with small scar formation characterizes stage V at six weeks to several months following infestation. More severe cases may also present with dystrophy or loss of the toenail, and/or permanently deformed toes [8].
Treatment involves extraction of the flea from the wound with a sterile needle followed by a sterile saline wash. With Stage III or later lesions, excision by deep shave followed by curettage with hyfrecation will suffice. Topical antibiotics should be applied to the area postoperatively. To date, no uniformly effective anti-parasitic drug has been identified to treat this particular entity. Although often effective against a broad range of ectoparasites, ivermectin did not show better efficacy than a placebo in a randomized, double-blind, controlled trial utilizing a relatively high dosage (2 x 300ug/kg) [9]. When secondary infections occur, culture most commonly reveals Staphylococcus aureus or various enterobacteriaceae [10]. If secondary infection is suspected, appropriate oral antibiotics should be administered. Other rare infectious complications of this disease may include gas gangrene, tetanus, and septicemia [9]. Generally however, prognosis is very good if sterile methods are employed during flea extraction and there is no pre-existing secondary infection.
Because T. penetrans primarily inhabits regions of South and Central America, sub-Saharan regions of Africa, and India, the general North American populace is not at high risk. Virtually all cases observed in the United States, Canada and Northern Europe involve history of travel to a high-risk country [11, 12]. Walking in the sand of these areas with bare feet or sandals significantly increases the risk of contracting this parasite. Close contact with dogs, cats or other domestic/farm animals, which serve as vectors in these regions, may also increase the risk of transmission. Persons traveling to infested areas should be counseled to wear shoes and insect repellent at all times.
References
1. Muehlen M, Heukelbach J, Wilcke T et al Investigations on the biology, epidemiology, pathology and control of Tunga penetrans in Brazil II. Prevalence, parasite load and topographic distribution of lesions in the population of a traditional fishing village. Parasitol Res 2003;90(60):449-455. PubMed2. Hoeppli R. Early references to the occurrence of Tunga penetrans in tropical Africa. Acta Trop. 1963;20:143-53. PubMed
3. Sachse MM , Guldbakke KK, Khachemoune A. Tunga penetrans: A stowaway from around the world J Eur Acad of Dermat Venereol 2007;21 (1):11-16 PubMed
4. Eisele M, Heukelbach J, Van Marck E, et al. H Investigations on the biology, epidemiology, pathology and control of Tunga penetrans in Brazil: I. Natural history of tungiasis in man. Parasitol Res 2003;90(2):87-99. PubMed
5. Bezerra Sm. Tungiasis: An unusual case of severe infestation. Int J Derm 1994;33(10): 725. PubMed
6. Veraldi S, Camozzi S, Scarabelli G. Tungiasis presenting with sterile pustular lesions of the hand. Acta Derm Venereol 1996;76(6):495. PubMed
7. Bakos Rm, Bakos L. "Whitish chains" A remarkable in vivo dermoscopic finding of tungiasis. Br J Dermatol 2008;159(4):991-2. PubMed
8. Kehr JD, Heukelbach J, Mehlhorn H, Feldmeier H Morbidity assessment in sand flea disease (tungiasis). Parasitol Res 2007:100(2):413-421. PubMed
9. Heukelbach J, Franck S, Feldmeier H. Therapy of tungiasis: a double-blinded randomized controlled trial with oral ivermectin. Mem Inst Oswaldo Cruz. 2004;99(8):873-6. PubMed
10. Feldmeier H, Heukelbach J, Eisele M, et al. Bacterial superinfection in human tungiasis Trop Med Int Hlth 2002;7(7): 559-564. PubMed
11. Veraldi S, Valsecchi M (2007) Imported tungiasis: a report of 19 cases and review of the literature. Int J Dermatol 2007; 46(10):1061-1066. PubMed
12. Leung AKC, Woo T, Robson WLM, Trotter MJ. A tourist with tungiasis. CMAJ. 2007;177(4):343-344. PubMed
© 2008 Dermatology Online Journal