Osseous metaplasia late in the course of nephrogenic systemic fibrosis
Published Web Location
https://doi.org/10.5070/D34jv4h6z9Main Content
Osseous metaplasia late in the course of nephrogenic systemic fibrosis
David R Berk MD, Alicia Miller MD, Debra Scarlett MD, Franz J Wippold II MD, Susan J Bayliss MD, Dongsi Lu MD PhD
Dermatology Online Journal 16 (8): 3
Department of Internal Medicine, Division of DermatologyDepartment of Pathology and Immunology
Mallinckrodt Institute of Radiology Washington University School of Medicine
St. Louis, Missouri. dberk@dom.wustl.edu
Abstract
Osseous metaplasia has recently been described in several cases of nephrogenic systemic fibrosis, sometimes in association with unusual clinical features such as painful hyperkeratotic spicules, palpable bony masses, and disease regression. Some authors have suggested that it may mainly occur late in the disease course or even be a marker for involuting nephrogenic systemic fibrosis. Here, we present a 27-year-old woman with a 7-year history of nephrogenic systemic fibrosis, who developed cutaneous osseous metaplasia.
Introduction
Recently, several reports of patients with nephrogenic systemic fibrosis (NSF) and histological evidence of cutaneous [1-3] or extracutaneous [4, 5] osseous metaplasia have appeared in the literature. The significance of this rare histological finding remains uncertain. Clinically, the development of osseous metaplasia in NSF has been correlated with various findings, such as new painful hyperkeratotic spicules [1], palpable bony masses [5], and softening of previously indurated plaques [1]. However, several other cases have apparently not demonstrated any obviously unusual clinical features [3]. Some authors have suggested that osseous metaplasia primarily develops in longstanding lesions of NSF late in the course of the disease [1, 2, 5] or may even be a marker for involuting or resolving NSF [1, 2]. Cases of osseous metaplasia in NSF have demonstrated histological features reminiscent of NSF (e.g., increased and thickened collagen, spindle cells, stromal mucin, sparse inflammatory infiltrate), as well as islands and spicules of variably mineralized woven bone, often containing fragmented elastic fibers. Variable features include calcification (sparing vasculature), osteoblasts, osteoclasts, “elastocollagenous balls” [2], and transepidermal elimination [1]. Histologically, osseous metaplasia in NSF should be distinguished from collagenous sclerotic bodies with entrapped elastic fibers, another recently reported rare finding in NSF [6]. As in other examples of secondary osteoma cutis, the pathogenesis of osseous metaplasia in NSF remains uncertain.
Here, we present a 27-year-old woman with systemic lupus erythematosus, nephritis, dialysis-dependent renal failure, and a 7-year history of NSF who was found to have osseous metaplasia in those biopsies taken late but not early in the course of her disease. This case further supports the notion that osseous metaplasia tends to mainly occur later in the course of disease, many years after clinical onset of NSF. However, the presentation and several years of follow-up of the present case do not support the idea that osseous metaplasia is a marker of involuting NSF or necessarily correlates with unusual clinical features.
Case report
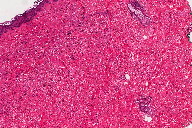
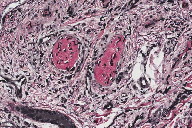
A 20-year-old Caucasian woman with a history of systemic lupus erythematosus complicated by chronic renal insufficiency secondary to diffuse proliferative glomerulonephritis, presented with a new onset of skin thickening on the arms and legs. Additional past medical history included pseudotumor cerebri, malignant hypertension, deep venous thrombosis, avascular necrosis of the knee, osteomyelitis of the foot, seizures, irritable bowel syndrome, depression, polysubstance abuse, hyperlipidemia, and hypothyroidism. Physical examination revealed skin-colored indurated plaques on the arms and legs. Punch biopsies from both arms (Figure 1) revealed a dermal interstitial process with a minimal mononuclear inflammatory component demonstrated by a paucity of staining for CD45. Vimentin staining revealed a diffuse increase in spindled stromal cells presumably representing fibroblasts, with few if any histiocytes in the dermis as indicated by CD68 immunostaining. Colloidal iron staining revealed markedly increased dermal mucin. Direct immunofluorescence showed a linear granular pattern of deposition of IgG and C3 in the basement membrane zone, representing her systemic lupus erythematosus. The differential diagnosis at the time included scleromyxedema and interstitial granuloma annulare. Later that year, after publication of the first descriptions of the condition then known as nephrogenic fibrosing dermopathy [7], she was correctly diagnosed with NSF. Therapeutic trials with plaquenil and quinacrine were unsuccessful. Over the next 6 years, her renal disease worsened, requiring hemodialysis and ultimately a matched living-related kidney transplantation. Her NSF plaques remained generally stable. Six months after transplantation, she presented again to the dermatology service, this time because of concern about a drug eruption. She had a 1-week history of a new red pruritic rash on her legs, which began 2 days after starting pregabalin. Physical examination revealed skin-colored indurated plaques on the extremities and a few scattered erythematous papules on the legs. Within the indurated plaques, there were whitish-yellow, firm, angulated nodules with a positive “tent sign” as seen with pilomatricomas. There were no joint contractures.
 |
| Figure 2C |
|---|
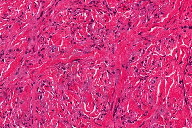
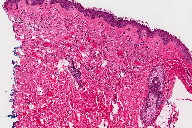
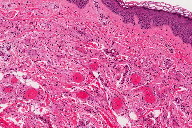
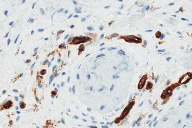
Because of the atypical clinical appearance and the interval change in the clinical appearance, 2 punch biopsies (Figure 2) were taken from nodular areas on the right leg. They demonstrate mild dermal fibrosis with increased number of fibroblasts and increased dermal mucin, consistent with NSF. In addition, there are multiple small, round collections of eosinophilic material with surrounding fibrosis in the superficial and mid dermis, consistent with osteomas. There are flattened cells surrounding the osteomas, consistent with osteoblasts. Adjacent small vessels are unremarkable. CD31 staining shows that the surrounding cells to be negative and confirms the extravascular location of the osteomas. There are short hyphae-like material within the osteomas, and Verhoeff-Van Gieson stain demonstrates that they are positive-stained elastic fibers. Von Kossa stain shows no apparent calcium deposition.
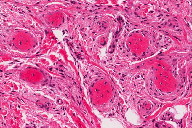
Her superimposed drug eruption resolving after discontinuing pregabalin. A subsequent 6-month trial of thalidomide did not improve her NSF. At follow-up 2 years later, her lesions have not significantly changed (Figure 3).
Discussion
Osteoma cutis is a rare phenomenon of uncertain pathogenesis characterized by the presence of mature osseous tissue in the dermis and/or subcutis. Osteoma cutis has traditionally been divided into primary and secondary forms (Table 1).[8, 9, 10] Secondary osteoma cutis is more common (approximately 75% of cases) than primary osteoma cutis, more common in females, and may be associated with various inflammatory, neoplastic, or traumatic processes, especially processes also prone to calcification. Benign neoplasms, such as melanocytic nevi and pilomatricomas, may be the most commonly associated processes. Among the inflammatory processes complicated by osteoma cutis are several connective tissue diseases including scleroderma and dermatomyositis. The clinical presentation of osteoma cutis is variable and dependent upon the type and extent of the condition, but may include local pain and disfigurement. Evaluation of patients with osteoma cutis should include consideration of underlying causes or associated syndromes, including history of enhanced MR imaging studies. Determination of serum calcium and phosphate may help to rule out an underyling metabolic abnormality. Serum parathyroid hormone level, vitamin D level, and 24-hour urinary calcium excretion may also be helpful. Treatment is frequently unsatisfactory and recurrence is common. Depending upon the type, extent, and symptoms, excision, dermabrasion, or topical retinoids may be therapeutic options.
Nephrogenic systemic fibrosis is a recently recognized [11] systemic disorder occurring primarily in patients with renal failure and usually with a history of receiving gadolinium-containing MR contrast agents [12]. Clinically, patients develop scleroderma-like cutaneous induration, which is typically progressive, often painful, worse on the extremities, sparing of the face, and associated with hyperpigmentation and contractures. Histologically, NSF closely resembles scleromyxedema, with increased collagen deposition, a spindle cell proliferation, and increased interstitial mucin. However, findings often involve the entire dermis and affect the subcutis, whereas scleromyxedema may be more limited to the upper and mid-dermis. Spindle cells include dual procollagen and CD34-positive cells. Other features include a sparse inflammatory infiltrate, increased elastic fibers, multinucleate giant cells, and dystrophic calcification. Rare histological features can include osteoclast-like giant cells [13], elastolysis [14], calciphylaxis-like vascular calcification [15], and pseudoxanthoma elasticum-like calcified fragmented elastic fibers [16].
Recently, cutaneous osseous metaplasia in NSF has been described in 3 reports describing a total of 4 patients (Table 2) [1, 2, 3]. This phenomenon was first reported by Ruiz-Genao et al. in 2005, in a 44-year-old man who clinically presented with painful, hyperkeratotic spicules in his popliteal fossae, which began 5 months after the onset of his NSF. Interestingly, the spicules appeared very shortly after the induration of his NSF spontaneously resolved. Biopsies revealed islands and spicules of variably mineralized woven bone in the superificial dermis, containing fragmented elastic fibers and located both parallel to and perforating the epidermal surface. Surrounding osteoblasts and osteoclasts were present. Concomitant histological findings more typical of NSF, including fibrosis, vascular proliferation, and a lympho-plasmacytic infiltrate were also demonstrated. Earlier biopsies of the indurated plaques, which preceded the clinical spicules, showed more classical findings of NSF, including a proliferation of CD34-positive fibroblast-like cells, interstitial mucin, and thick collagen bundles.
The subsequent 2 reports [2, 3] of osseous metaplasia in NSF did not include the painful hyperkeratotic spicules or perforating epidermal changes of the patient of Ruiz-Genao et al. First, Wiedemeyer et al. [2] described a 56-year-old man with hypertension, angiotensin converting enzyme inhibitor usage, focal glomerulosclerosis, dialysis-dependent renal failure, and an 8-year history of NSF manifesting blotchy red-brown macules and patches on the extremities. Biopsy of early lesions showed typical histologic features of NSF (increased collagen, CD34+ procollagen I+ spindle cells, and mucin), whereas biopsy of longstanding lesions showed scar-like fibrosis, refractile elastic fibers surrounded by course collagen strands (forming structures referred to as “elastocollagenous balls”), and osseous metaplasia in the superficial dermis, with more classical findings of NSF in the deep dermis and subcutaneous septae. On scanning electron microscopy with energy-dispersive x-ray spectroscopy, gadolinium was undetectable in the areas of elastocollagenous balls and osseous metaplasia but present in the deeper and/or more classic histological areas of NSF. The authors [2] hypothesized that the elastocollagenous balls and osseous metaplasia “may represent a late, involuting stage of NSF.” Finally, Deng et al. [3] presented 2 patients with NSF and cutaneous osseous metaplasia, including a 51-year-old woman with dialysis-dependent renal failure due to hypertension and a 2-year history of NSF and a 20-year-old woman with hepatic-renal syndrome and a 2-month history of NSF. Clinically, both patients had typical findings of NSF, including pigmented plaques on the extremities with variable pruritus, induration, and limitation of motion. Histologically, both patients demonstrated extensive dermal calcification and islands and spicules of mineralized and unmineralized woven bone in the upper and mid-dermis, without osteoblasts, osteoclasts, or vascular calcification. No subsequent evaluations were provided for the patients of either Wiedemeyer et al. or Deng et al.
Several reports of extracutaneous osseous metaplasia in patients with NSF have been published [4, 5]. Krous et al. [4] described a 15-year-old boy with a history of renal lymphoma, Ewing sarcoma, dialysis-dependent renal failure, NSF, headaches, and seizures, whose post-mortem findings included diffuse dural fibrosis and osseous metaplasia. Nagai et al. [5] described a 50-year-old man with an 8-year history of NSF who presented with severe disabling joint contractures and newly palpable bony masses over his legs. Biopsy of a large indurated nodule revealed dermal changes of NSF including increased and thickened collagen fibers with CD34-positive plump spindle cells. The fascial layer was thickened and fibrotic, with underlying osseous metaplasia and degenerated muscle fibers. Attempts at treatment with psoralen + UVA and sodium thiosulphate were unsuccessful.
Osseous metaplasia in NSF can closely resemble sclerotic bodies, a rare recently reported histological feature of NSF [6]. Bhawan et al. described 2 cases of NSF, which demonstrated dermal sclerotic bodies with entrapped elastic fibers in the dermis. The sclerotic bodies were thought to represent calcified hyalinized collagen. The authors highlighted this feature as a novel diagnostic clue for NSF. Like osseous metaplasia, the sclerotic bodies contained entrapped elastic fibers. Unlike osseous metaplasia, the sclerotic bodies lacked lacunae or cells, were more irregular in size and shape, and stained blue not red on Masson trichrome stain.
Further reports are needed to clarify the pathogenesis and significance of osseous metaplasia in NSF. In summary, cases of osseous metaplasia previously reported, including the present case, suggest that it may occur late in the course of NSF and may appear in the skin or extracutaneous tissue in patients with either typical or atypical clinical features (e.g., hyperkeratotic spicules, bony masses, whitish nodules) for NSF.
References
1. Ruiz-Genao DP, Pascual-Lopez MP, Fraga S, Aragues M and Garcia-Diez A. Osseous metaplasia in the setting of nephrogenic fibrosing dermopathy. J Cutan Pathol 2005;32:172-5. [PubMed]2. Wiedemeyer K, Kutzner H, Abraham JL, et al. The evolution of osseous metaplasia in localized cutaneous nephrogenic systemic fibrosis: a case report. Am J Dermatopathol 2009;31:674-81. [PubMed]
3. Deng A, Bilu Martin D, Spillane A, et al. Nephrogenic systemic fibrosis with a spectrum of clinical and histopathological presentation: a disorder of aberrant dermal remodeling. J Cutan Pathol 2009;37(2):204-10. [PubMed]
4. Krous HF, Breisch E, Chadwick AE, Pinckney L, Malicki DM and Benador N. Nephrogenic systemic fibrosis with multiorgan involvement in a teenage male after lymphoma, Ewing's sarcoma, end-stage renal disease, and hemodialysis. Pediatr Dev Pathol 2007;10:395-402. [PubMed]
5. Nagai Y, Hasegawa M, Shinmi K, et al. Nephrogenic systemic fibrosis with multiple calcification and osseous metaplasia. Acta Derm Venereol 2008;88:597-600. [PubMed]
6. Bhawan J, Swick BL, Koff AB and Stone MS. Sclerotic bodies in nephrogenic systemic fibrosis: a new histopathologic finding. J Cutan Pathol 2009;36:548-52. [PubMed]
7. Cowper SE, Su LD, Bhawan J, Robin HS and LeBoit PE. Nephrogenic fibrosing dermopathy. Am J Dermatopathol 2001;23:383-93. [PubMed]
8. Touart DM, Sau P. Cutaneous deposition diseases. Part II. J Am Acad Dermatol 1998;39:527-44; quiz 545-6. [PubMed]
9. Conlin PA, Jimenez-Quintero LP and Rapini RP. Osteomas of the skin revisited: a clinicopathologic review of 74 cases. Am J Dermatopathol 2002;24:479-83. [PubMed]
10. Roth SI, Stowell RE and Helwig EB. Cutaneous ossification. Report of 120 cases and review of the literature. Arch Pathol 1963;76:46-56. [PubMed]
11. Cowper SE, Robin HS, Steinberg SM, Su LD, Gupta S and LeBoit PE. Scleromyxoedema-like cutaneous diseases in renal-dialysis patients. Lancet 2000;356:1000-1. [PubMed]
12. Grobner T. Gadolinium--a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol Dial Transplant 2006;21:1104-8. [PubMed]
13. Hershko K, Hull C, Ettefagh L, et al. A variant of nephrogenic fibrosing dermopathy with osteoclast-like giant cells: a syndrome of dysregulated matrix remodeling? J Cutan Pathol 2004;31:262-5. [PubMed]
14. Glaich AS, Martinelli PT, Markus RF and Hsu S. Generalized elastolysis following nephrogenic fibrosing dermopathy. J Am Acad Dermatol 2005;53:174-6. [PubMed]
15. Edsall LC, English JC, 3rd, Teague MW and Patterson JW. Calciphylaxis and metastatic calcification associated with nephrogenic fibrosing dermopathy. J Cutan Pathol 2004;31:247-53. [PubMed]
16. Lewis KG, Lester BW, Pan TD and Robinson-Bostom L. Nephrogenic fibrosing dermopathy and calciphylaxis with pseudoxanthoma elasticum-like changes. J Cutan Pathol 2006;33:695-700. [PubMed]
© 2010 Dermatology Online Journal