Erosive pustular dermatosis of the scalp after photodynamic therapy
Published Web Location
https://doi.org/10.5070/D333b9s5wbMain Content
Erosive pustular dermatosis of the scalp after photodynamic therapy
Verónica López1 MD, Inmaculada López1 MD, Virginia Ramos2 MD, José M Ricart1 MD
Dermatology Online Journal 18 (9): 13
1. Department of Dermatology2. Department of Pathology
Dermiláser Hospital Quirón de Valencia, Valencia, Spain
Abstract
Erosive pustular dermatosis of the scalp is a rare condition that tends to occur mainly in elderly patients. Clinically it is characterized by the presence of pustules, chronic crusted erosions with progressive scarring alopecia, and skin atrophy. Although etiology remains unclear, it seems to be triggered by local trauma such as surgical procedures, skin graft, ultraviolet light exposure, cryotherapy, craniotomy, or radiotherapy. To our knowledge, erosive pustular dermatosis of the scalp after photodynamic therapy has been seldom reported. We described a 81-year-old woman presenting with erosive pustular dermatosis of the scalp after photodynamic therapy for actinic keratosis.
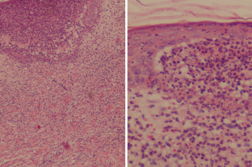
An 81-year-old woman, with no relevant medical history, was seen for evaluation of multiple actinic keratoses on the scalp previously treated with cryotherapy and topical imiquimod. Treatment with topical methylaminolaevulinate photodynamic therapy was suggested. Thus, scales and hyperkeratoses removal with a curette was followed by the application of methylaminolaevulinate cream for 3 hours under occlusion and irradiation with a dose of 37J/cm² of red light for 9 minutes. A second session was performed one month later. After treatment, no actinic keratosis was observed. However, three months later, the patient presented again at our clinic with a three-week history of multiple erosions, pustules, scales, and crusts on the scalp that started as multiple isolated small pustules that progressively developed into large and confluent erosive plaques with crusts (Figure 1). A blood test and bacterial and mycological cultures from the scalp were normal. Histopathological examination from one of the lesions showed subcorneal neutrophilic pustules and diffuse infiltrate of primarily neutrophils within the papillary dermis associated with edema and hemorrhage (Figure 2). Based on the clinicopathological findings, a diagnosis of erosive pustular dermatosis was established. Treatment included mometasone furoate cream twice a day for one week, followed by tacrolimus ointment twice a day for one month resulting in a significant improvement of the condition. After a 4-month follow-up, scarring alopecia was observed but no signs of relapse were present.
Erosive pustular dermatosis of the scalp (EPDS) is a rare condition characterized by the presence of pustules, chronic crusted erosions, progressive scarring alopecia, and skin atrophy [1]. It tends to occur mainly in elderly patients, with a female predominance. Although the etiology remains unclear, it seems to be triggered by local trauma such as surgical procedures, skin graft, ultraviolet light exposure, cryotherapy, craniotomy, or radiotherapy. Furthermore, autoimmune disorders and actinic damage have been associated with EPDS [2, 3]. To our knowledge, only two cases of EPDS after photodynamic therapy for actinic keratosis have been reported [2]. The mean interval between onset of the trigger factor and EPDS presentation is variable, ranging from 1 to 55 months [1]. Clinically, it presents as pustules and erosive, crusted plaques with a purulent exudate on the scalp, with occasional extension onto the face. Lesions may resolve leading to scarring alopecia and skin atrophy.
Histologic findings are nonspecific and include parakeratosis or hyperkeratosis, ulceration or atrophy of the epidermis, inflammatory dermal infiltrate of lymphocytes and plasma cells, and reduced or absent hair follicles [4].
The diagnosis of EPDS is made after excluding many other entities in the differential diagnosis including folliculitis decalvans, bacterial folliculitis, kerium, impetiginized eczema, pustular psoriasis, subcorneal pustular dermatosis, pyoderma gangrenosum, autoimmune blistering disorders, squamous cell carcinoma, temporal arteritis, halogenoderma, and dermatitis artefacta [4].
Treatment includes potent topical steroids, calcipotriol cream, tacrolimus ointment, and oral treatments with isotretinoin, dapsone, zinc sulphate, and nimesulide [5].
In summary, we have reported the third case of EPDS that developed after photodynamic therapy and we underscore the importance of including this disorder in the differential diagnosis of pustular dermatosis of the scalp, especially if a previous history of trauma and significant actinic damage are present.
References
1. Mastroianni A, Cota C, Ardigò M, Minutilli E, Berardesca E. Erosive pustular dermatosis of the scalp: a case report and review of the literature. Dermatology 2005: 211:273-76. [PubMed]2. Guarneri C, Vaccaro M. Erosive pustular dermatosis of the scalp following topical methyaminolaevulinate photodynamic therapy. J Am Acad Dermatol 2009; 3:521-22. [PubMed]
3. Skellett AM, Levell NJ. Erosive pustular dermatosis and osteoradionecrosis: complications of radiotherapy. Clin Exp Dermatol. 2011;36:98-9. [PubMed]
4. Van Exel CE, English JC. Erosive pustular dermatosis of the scalp and nonscalp. J Am Acad Dermatol 2007; 57(2 Suppl):511-4. [PubMed]
5. Darwich E, Muñoz-Santos C, Mascaró JM. Erosive pustular dermatosis of the scalp responding to acitretin. Arch Dermatol. 2011;147:252-3. [PubMed]
© 2012 Dermatology Online Journal