Pellagra as the initial presentation of Crohn disease
Published Web Location
https://doi.org/10.5070/D30rd7m740Main Content
Letter: Pellagra as the initial presentation of Crohn disease
Aristóteles Rosmaninho, Madalena Sanches, Iolanda Conde Fernandes, Teresa Pinto-Almeida, Susana Vilaça, Ana Oliveira, Manuela
Selores
Dermatology Online Journal 18 (4): 12
Dermatology Department, Centro Hospitalar do Porto, EPE-HSA, Porto, PortugalAbstract
Pellagra is a nutritional disease caused by the deficiency of niacin. We describe a case of pellagra as the initial presentation of Crohn disease, which has been rarely described in the literature.
Introduction
In western countries, pellagra is rarely seen and is confined to individuals who have improper food intake such as psychiatric patients or alcoholics and patients with malabsorptives states [1]. We report a case of pellagra as the initial presentation of Crohn disease in a 57-year-old female.
Case report
A 57-year-old woman presented for evaluation of a 3-week history of a skin rash involving her hands and feet. On physical examination a symmetric bright scaly erythematous-brown eruption was observed on the dorsum of the hands and feet. On the feet the lesions took on the configuration of her open shoes. Bullae at the calcaneal area as well as glossitis and marked edema of the lower legs were also present.
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Symmetric bright scaly erythematous-brown eruption on the hands. Figure 2. Symmetric scaly eruption on the feet. | |
 |  |
| Figure 3 | Figure 4 |
|---|---|
| Figure 3. Bullous lesions at calcaneal area. Figure 4. Marked edema of the lower leg. | |
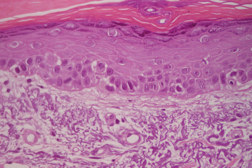
The skin lesions had a photosensitive distribution and were painful to touch. She complained about anorexia, fatigue, irritability, and watery diarrhea in the last 2 months. She had no medical history of inflammatory bowel disease. However, she complained about episodic abdominal pain, diarrhea, and a weight lost of 20 kg during the last 4 years. She was being treated with omeprazole for several years and denied the intake of other drugs. Analytical studies revealed a normocytic normochromic anemia with hemoglobin of 9.2 g/dl (normal: >12), severe hypoproteinemia and hypoalbuminemia with total serum proteins of 3.0 g/dl (normal: >6.0) and albumin of 0.8 g/dl (normal: >3.5), respectively. In addition, serum transferrin of 37 mg/dl (normal: >200), potassium of 3.1 mmol/l (normal: >3.5) and calcium of 2.9 mmol/l (normal: <2.4) were documented. HIV serology was negative. A skin biopsy from the dorsum of the hand was performed and showed slight atrophy of the epidermis with orthokeratotic hyperkeratosis and dermal elastolysis with a discrete inflammatory infiltrate.
 |
| Figure 5 |
|---|
| Figure 5. Slight atrophy of the epidermis with orthokeratotic hyperkeratosis and dermal elastolysis with a discrete inflammatory infiltrate (H&E, x40). |
All the above findings were consistent with the diagnosis of pellagra. Endoscopic evaluation showed the presence of bulbus stenosis and ileal ulcers; a biopsy showed noncaseating granulomas, confirming the patient to have Crohn disease.
The patient was treated with albumin infusions and started on oral multivitamin supplementation that contained 200 mg of niacin daily. Crohn disease was managed with oral prednisolone 1 mg/kg daily and oral metronidazole 1 g daily. Skin lesions disappeared within 2 weeks after niacin supplementation was initiated.
Discussion
Pellagra is a nutritional disease caused by the deficiency of niacin. It is a clinical syndrome characterized by 4 “D’s”: diarrhea, dermatitis, dementia, and ultimately death [2]. Secondary pellagra can occur as a consequence of prolonged diarrhea, anorexia nervosa, chronic alcoholism, chronic colitis, regional ileitis, carcinoid tumor, Hartnup disease, HIV disease, or medications such as 5-fluorouracil, pyrazinamide or anticonvulsant drugs, among others [3, 4]. The dermatitis is a characteristic bilaterally symmetrical eruption at cutaneous sites of solar exposure and tends to be painful to touch during the acute phase [5]. The back of the hands is the most common area involved. The photosensitivity reaction may be the result of a deficiency of urocanic acid and/or cutaneous accumulation of kynurenic acid [2]. When the cutaneous findings are present they are pathognomonic of the disease. However, if the cutaneous features are absent it may go unrecognized. The diagnosis should focus on the presence of the 3 “D’s” and there are no chemical tests available to definitively diagnose pellagra [2, 5]. Low levels of serum niacin, tryptophan, NAD and NADP, and low levels of the urinary metabolites of N'-methyl-nicotinamide and N'-methyl-2-pyrindone-5-carboxamide are highly suggestive of the diagnosis [2]. However, they aren’t currently available in most laboratories (as in our case). A rapid improvement of the skin lesions with niacin supplementation also favors the diagnosis. Early neurologic symptoms may be misinterpreted and include insomnia, depression, or fatigue [2, 6]. In pellagra, pathological changes in the skin are relatively nonspecific. Vesicles may be seen in the initial cutaneous lesions as a result of vacuolar degeneration of the basal layer (also present in acrodermatitis enteropathica and necrolytic eythema). This stage is followed by acanthosis with hyperkeratosis of the epidermis and in older lesions the process is characterized by atrophy of the epidermis with flattening of the rete ridges and a chronic inflammatory infiltrate. A review of the literature confirms the paucity of reports of the dermatosis as a complication of Crohn disease. It is even rarer as the initial manifestation of this inflammatory disease [7, 8]. Because the disease is exceptional in developed countries, the degree of clinical suspicion is likely to be low; physicians must be able to recognize this entity.
References
1. Nogueira A, Duarte AF, Magina S, Azevedo F. Pellagra associated with esophageal carcinoma and alcoholism. Dermatol Online J. 2009 May 15;15(5):8. [PubMed]2. Hegyi J, Schwartz RA, Hegyi V. Pellagra: dermatitis, dementia, and diarrhea. Int J Dermatol 2004 Jan;43(1):1-5. [PubMed]
3. Stratigos JD, Katsambas A. Pellagra: a still existing disease. Br J Dermatol 1977;96:99-106. [PubMed]
4. Lyon VB, Fairley JA. Anticonvulsant-induced pellagra. J Am Acad Dermatol 2002 Apr;46(4):597-9. [PubMed]
5. Karthikeyan K, Thappa DM. Pellagra and skin. Int J Dermatol 2002 Aug;41(8):476-81. [PubMed]
6. Adams RD, Victor M, Ropper AH. Principles of Neurology. In: Diseases of the nervous system due to nutritional deficiency (Adams RD, Victor M, Ropper AH, eds), 6th edn. New York: McGraw-Hill 1997:1138-1165.
7. Zaki I, Millard L. Pellagra complicating Crohn's disease. Postgrad Med J 1995 Aug;71(838):496-7. [PubMed]
8. Lifshitz AY, Stern F, Kaplan B, Sofer E, Sela BA, Schewach-Millet M. Pellagra complicating Crohn's disease. J Am Acad Dermatol 1992 Oct;27(4):620. [PubMed]
© 2012 Dermatology Online Journal

