Piebaldism in a 2-year-old girl
Published Web Location
https://doi.org/10.5070/D30546v775Main Content
Piebaldism in a 2-year-old girl
Verónica López MD, Esperanza Jordá MD PhD
Dermatology Online Journal 17 (2): 13
Departments of Dermatology, Hospital Clínico Universitario de Valencia, Valencia, SpainAbstract
Piebaldism is a rare autosomal dominant skin disorder characterized by a white forelock and depigmented patches of skin, generally located on the forehead, central chest and abdomen, upper arms, and lower extremities. We report a case of a 2-year-old girl with a typical presentation and review the literature concerning this condition.
Case report
 |  |
| Figure 1 | Figure 2 |
|---|---|
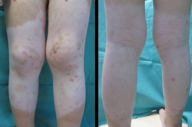
| Figure 1. Image showing depigmented patches over the trunk and upper extremities Figure 2. Image showing depigmented patches over the lower extremities | |
A 2-year-old girl, with no relevant medical history, was referred to our department for evaluation of a white forelock and white patches over the trunk, upper extremities and lower extremities. Her mother informed us that the white forelock was present since birth, whereas the white patches involving the central forehead, abdomen, and extremities had progressively appeared, but remained unchanged since they had developed. Her father exhibited a white forelock and similar lesions over the trunk.
 |
| Figure 3 |
|---|
| Figure 3. White forelock in our patient |
Physical examination showed a healthy girl with multiple irregularly shaped, depigmented macules over the trunk, upper extremities, and lower extremities (Figures 1 and 2). Several hyperpigmented macules were present within and at the border of the depigmented areas (Figures 1 and 2). Moreover, a white forelock of hair was observed (Figure 3). No axillary or inguinal freckling was noted. Neither nasal nor ophthalmic anomalies were observed; there was no deafness.
Based on this, a diagnosis of piebaldism was made. No treatment was given and during two-year follow-up the lesions have remained stable.
Discussion
Piebaldism is an autosomal dominant disorder characterized by the congenital absence of melanocytes in the affected areas of the hair and skin. This disorder is caused by mutations of the c-kit proto-oncogene, which encodes the tyrosine kinase transmembrane cellular receptor for the mast/stem cell growth factor [2]. The kit gene is related to melanoblast migration, proliferation, differentiation, and survival [3]. So, the site of mutation within this gene correlates with the severity of the phenotype in piebaldism. To date, 14 point mutations, 9 delections, 2 nucleotide splice mutations, and 3 insertions of the kit gene have been described in the literature [3]. Mutations in the c-kit gene are found in about 75 percent of patients affected with piebaldism. In patients that lack mutations in the c-kit gene, mutations in a zinc-finger neural crest transcription factor, the slug gene, have been described [4].
Clinically, piebaldism is characterized by stable and persistent, well-circumscribed depigmented patches present at birth affecting the skin of the face, trunk, and extremities in a symmetrical distribution [1]. Typically, hyperpigmented freckle-like macules may be observed within and at the border of depigmented areas. Dorsal midline, hands, feet, and periorificial areas are usually spared. Anomalies in the hair are observed. They are characterized by a white forelock of hair present in 80-90 percent of cases [5]. The eyebrows and eyelashes may also be affected in severe cases.
Piebaldism may be associated with other disorders such as Hirschprung disease or aganglionic megacolon, neurofibromatosis type I, congenital dyserythropoietic anemia type II, Diamond-Blackfan anemia, Grover disease, or transient acantholytic disease [5].
The diagnosis should be established to exclude other disorders clinically presenting with depigmentation or hypopigmentation of hair and skin, such as vitiligo and albinism [5]. Vitiligo is distinguished from piebaldism by the presence of unstable hypopigmented lesions that are acquired later in life. Albinism, an autosomal recessive disease, presents with widespread skin involvement and lacks the characteristic hyperpigmented macues within hypopigmented areas. In addition, there are usually significant hair and eye anomalies.
When other anomalies are present with hair and skin involvement, some syndromes should be ruled out. Waardenburg syndrome, an autosomal dominant disorder, is characterized by a congenital forelock, lateral displacement of the medial canthi, hypertrophic nasal root, partial or total heterochromia of the iris, and deafness [6]. Four types have been reported according to clinical and genetic criteria. Other syndromes associated with congenital deafness are Ziprkowski-Margolis syndrome and Woolf syndrome. The first is an X-linked recessive syndrome characterized by deaf-mutism, heterochromic irides, piebald-like hypomelanosis, and hyperpigmented macules over the trunk and extremities [5]. Woolf syndrome is an autosomal recessive disorder presenting with piebaldism and deafness [5].
Other conditions, including Addison disease, albinism, and systemic sclerosis can present with hypopigmentation, but can generally be easily distinguished. However, the use of depigmenting agents should be excluded [5].
Treatment of piebaldism is challenging. Topical treatment with make up or artificial pigmenting agents such as the tanning product dihydroxyacetone are useful, although temporary [7]. Sunscreens should be recommended to avoid sunburns and to reduce the carcinogenic potential.
Several surgical techniques are available for the treatment of stable leukoderma. These techniques include transfer of melanocytes by total or partial skin graft, minigrafting, or suction bubbles. Treatment with a combination of dermabrasion and grafting or a combination of Erbium:YAG laser surgery for disepithelialization and autologous cultured epidermal grafting on the recipient bed have been reported [8, 9, 10]. Recently, transplant of autologous melanocytes obtained through the culture of melanocytes or of melanocytes and keratinocytes has been described as a safe and effective treatment for patients with piebaldism. This induced scarless repigmentation using a small donor site [11, 12]. After these procedures, phototherapy can be used.
In conclusion, we have reported a typical case of piebaldism affecting a 2-year-old girl and a review of the literature of this condition.
References
1. Thomas I, Kihiczak G, Fox M, Janniger C, Schwartz R. Piebaldism: an update. Int J Dermatol 2004; 43:716-19. [PubMed]2. Spritz RA. Molecular basis of human piebaldism. J Invest Dermatol. 1994;103:137-140S. [PubMed]
3. Richards KA, Fukai K, Oiso N, et al. A novel KIT mutation results in piebaldism with progressive depigmentation. J Am Acad Dermatol. 2001; 44:288-92. [PubMed]
4. Sanchez-Martin M, Perez-Losada J, Rodriguez-Garcia A, et al. Deletion of th SLUG (SNAI2) gene results in human piebaldism. Am J Hum Genet. 2003; 122:125-32. [PubMed]
5. Janjua S, Khachemoune A, Guldbakke KK. Piebaldism: a case report and a concise review of the literature. Cutis. 2007; 80:411-14. [PubMed]
6. Waardenburg PJ. A new syndrome combining developmental anomalies of the eyelids, eyebrows and nose root with pigmentary defects of the iris and head hair and with congenital deafness. Am J Hum Genet. 1951; 3:195-253. [PubMed]
7. Suga Y, Ikejima A, Matsuba S et al. Medical pearl: DHA application for camouflaging segmental vitiligo and piebald lesions. J Am Acad Dermatol. 2002; 47:436-38. [PubMed]
8. Falabella R, Barona M, Escobar C et al. Surgical combination therapy for vitiligo and piebaldism. Dermatol Surg. 1995; 21: 852-57. [PubMed]
9. Njoo MD, Nieuweboer-Krobotova L, Westerhof W. Repigmentation of leucodermic defects in piebaldism by dermabrasion and thin split-thickness skin grafting in combination with minigrafting. Br J Dermatol. 1998; 139:829-33. [PubMed]
10. Guerra L, Primavera G, Raskovic D et al. Permanent repigmentation of piebaldism by erbium:YAG laser and autologous cultured epidermis. Br J Dermatol. 2004; 150:715-21. [PubMed]
11. van Geel N, Wallaeys E, Goh BK, De Mil M, Lambert J. Long-term results of noncultured epidermal cellular grafting in vitiligo, halo naevi, piebaldism and naevus depigmentosus. Br J Dermatol. 2010 Dec;163(6):1186-93. [PubMed]
12. Neves DR, Régis Júnior JR, Oliveira PJ, Zac RI, Silveira Kde S. Melanocyte transplant in piebaldism: case report. An Bras Dermatol. 2010 Jun;85(3):384-8. [PubMed]
© 2011 Dermatology Online Journal

